AUTHOR: JUDITH ANNE GOULD, BPHTY (HONS), MPHIL
- 9th Floor, 10 Pottinger Street, Central
- (852) 2167-8801
- reception@posture-plus.com
ONERO Exercise for Bone Health (Case Study)
- Home
- ONERO Exercise for Bone Health (Case Study)
The Effects of a Research-Based Exercise Program (Onero™) on Bone Mineral Density and Functional Measurements in Men and Women with Osteoporosis or Osteopenia in Hong Kong: A Case Study Series
INTRODUCTION
Osteoporosis and Osteopenia are common conditions amongst older adults in Hong Kong which can increase the risk of fractures and result in significant morbidity and mortality rates. A 2019 study estimated the prevalence of osteoporosis in people over the age of 50 in Hong Kong to be as high as 37%4. A more recent study in 2021 which focused on 1800 elderly women in Hong Kong (over 65) found that 15.9% were considered normal, 33.2% were low risk osteopenic, 27.2% were high-risk osteopenic and 23.7% were osteoporotic5.
High-intensity exercise has been shown to be an effective intervention to improve BMD and functional measurements in postmenopausal women and men over the age of 50 2,3,. However, there is limited research on the effectiveness of exercise interventions in younger people (under the age of 60) with osteopenia or osteoporosis in Hong Kong as most studies concentrate on postmenopausal women and men over 60 years of age6,7,8.
OBJECTIVES
This case study series aimed to report the potential benefits of a high-intensity exercise programme Onero™, on BMD in 4 clients (3 women and 1 man) and functional measurements of muscle strength, agility, and balance in 2 clients (1 woman and 1 man) with osteopenia or osteoporosis, all under the age of 60. The subjects were assessed and treated in a private physiotherapy clinic in Hong Kong by the same Physiotherapist.
METHODS
Subjects: Four subjects who had undergone a repeat DXA were chosen for review.
Client A
34-year-old female with osteoporosis of unknown origin
Client B
50-year-old perimenopausal female with osteopenia
Client C
59-year-old postmenopausal female breast cancer survivor w/ osteopenia and an atypical femoral fracture (AFF)
Client D
35-year-old old male with osteoporosis secondary to hyperparathyroidism
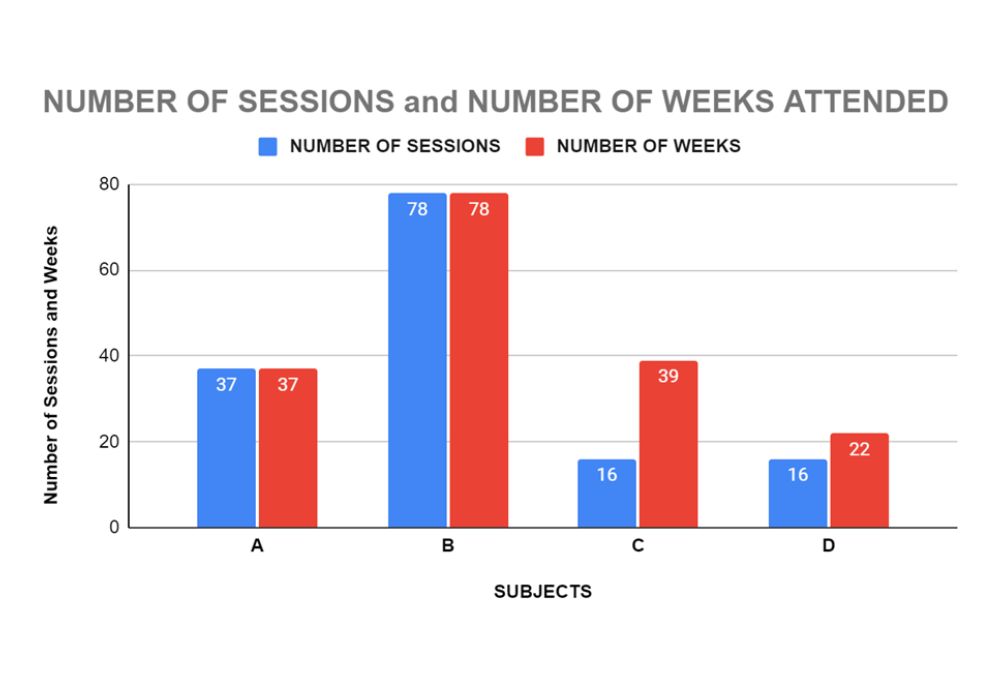
Exercise Intervention: Onero™ is a high-intensity resistance and impact training programme which consists of lifting weights, impact, and balance activities. The private sessions were 40 minutes in duration and clients attended a maximum of once a week for between 16 to 78 weeks (see graph 1 below)
Measurements: The before and after exercise intervention DXA tests were taken at various radiology clinics in HK (chosen by the individual client) and included different regions of interest (ROI). Each client was able to be retested at the same radiology clinic using the same equipment.
The functional measurements tested gait speed, lower extremity strength, and balance. Measurements included the following tests: tandem gait, 5 times sit to stand (5xSTS),functional reach (FR), Timed up and Go (TUG), Tragus to Wall (TTW), Knees to Wall (KTW),Single Leg Stance (SLST).
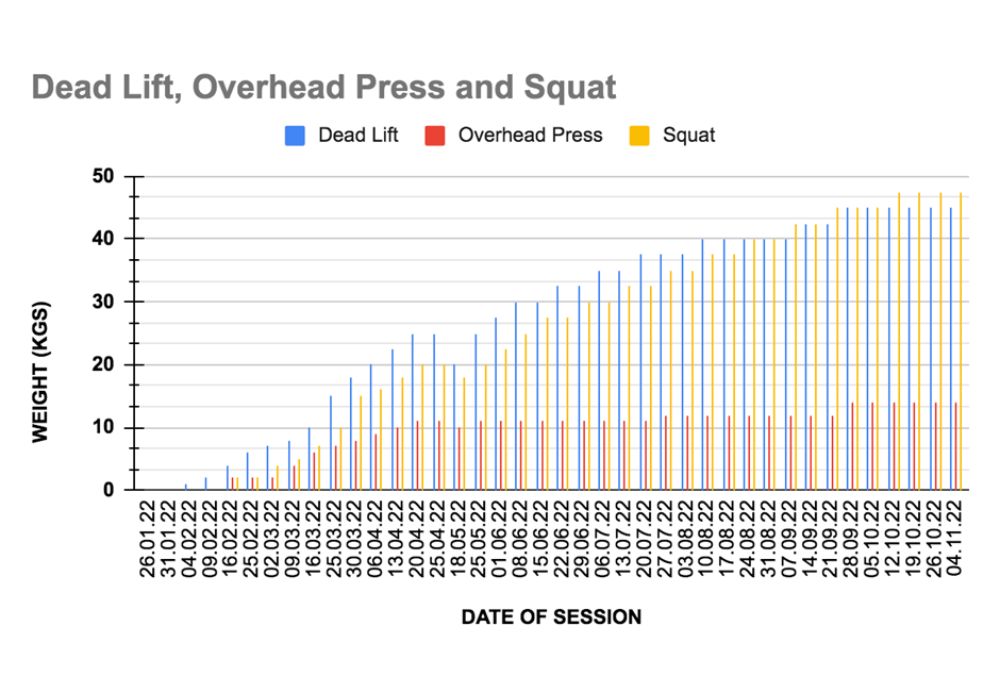
Exercise Progression: The exercises were progressively increased in intensity and difficulty over the course of the program according to the subject’s capabilities.
Graph 2 shows the progression of weights lifted by Subject A over the course of her treatment.
RESULTS
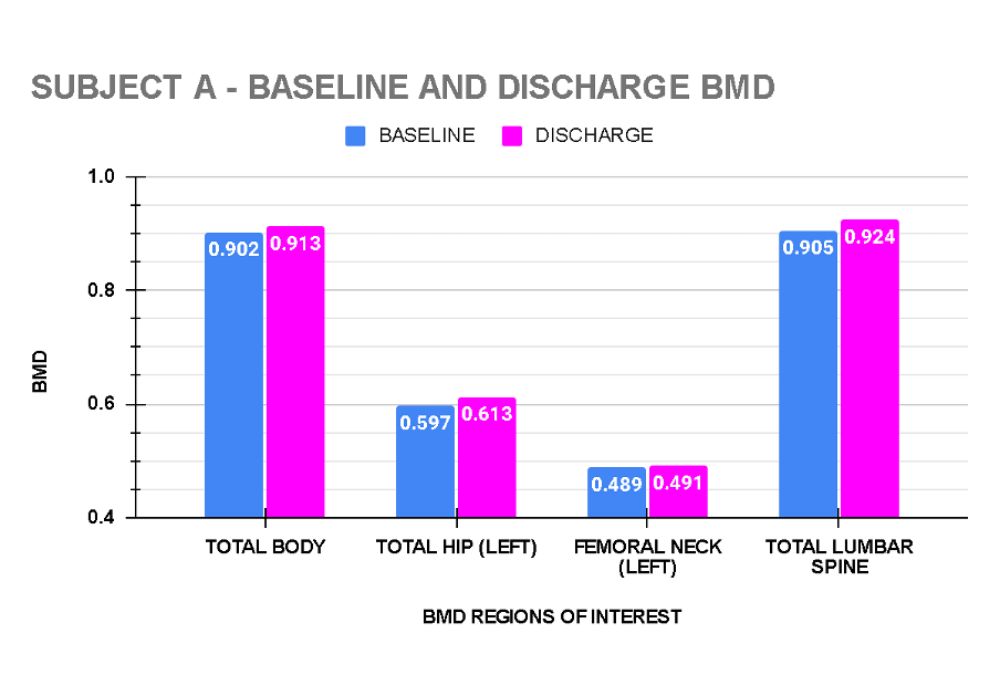
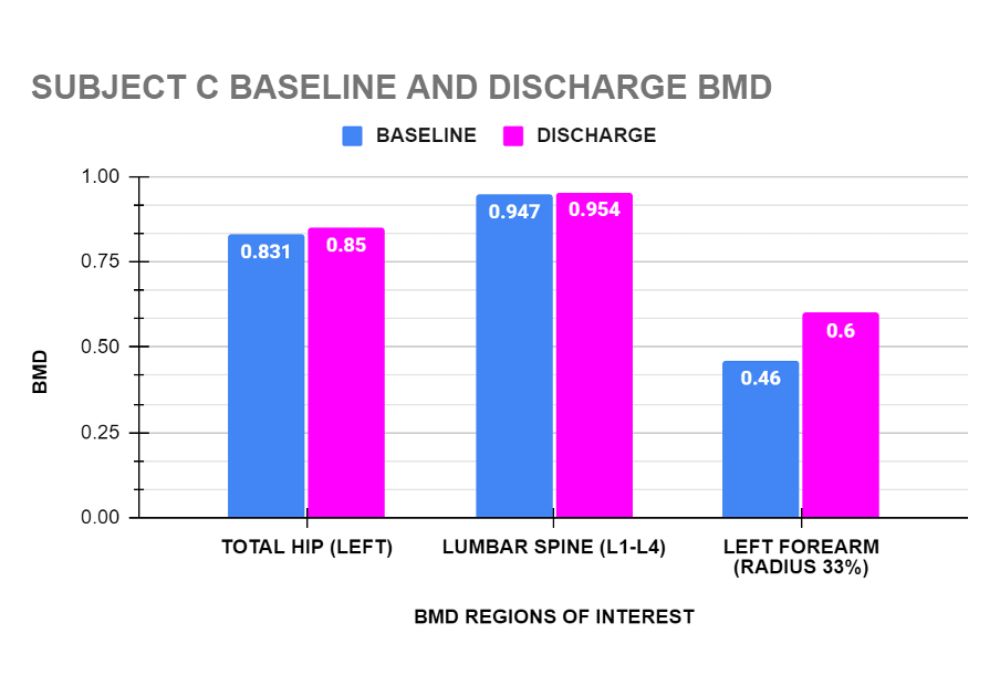
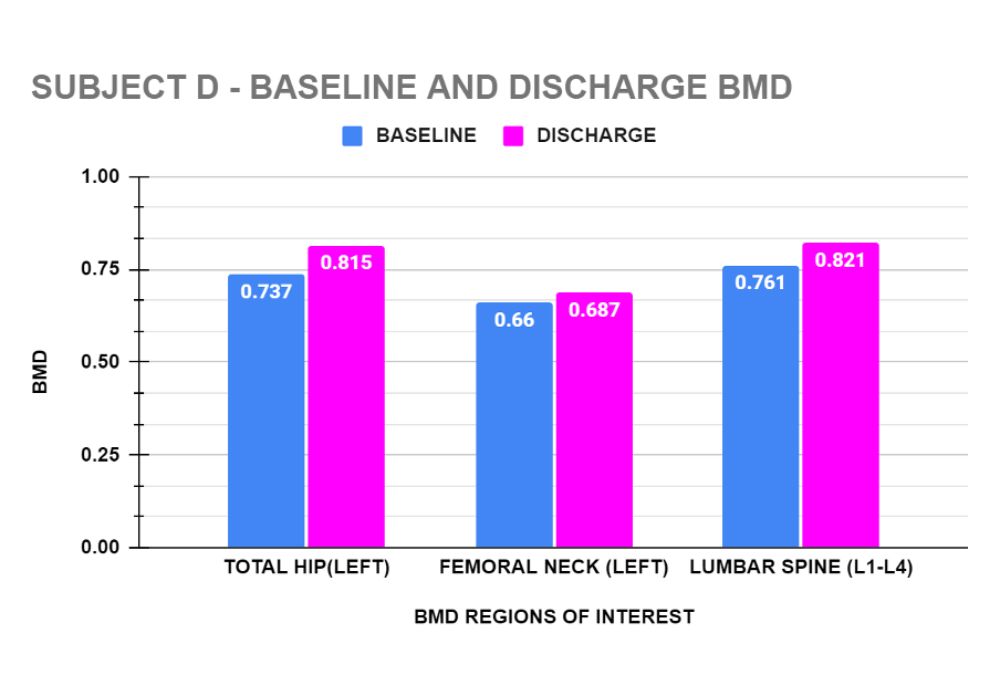
Graphs 3 to 6 show the baseline and end of treatment Bone Mineral Density measurements for each Subject A,B,C, and D respectively.
Functional Tests:
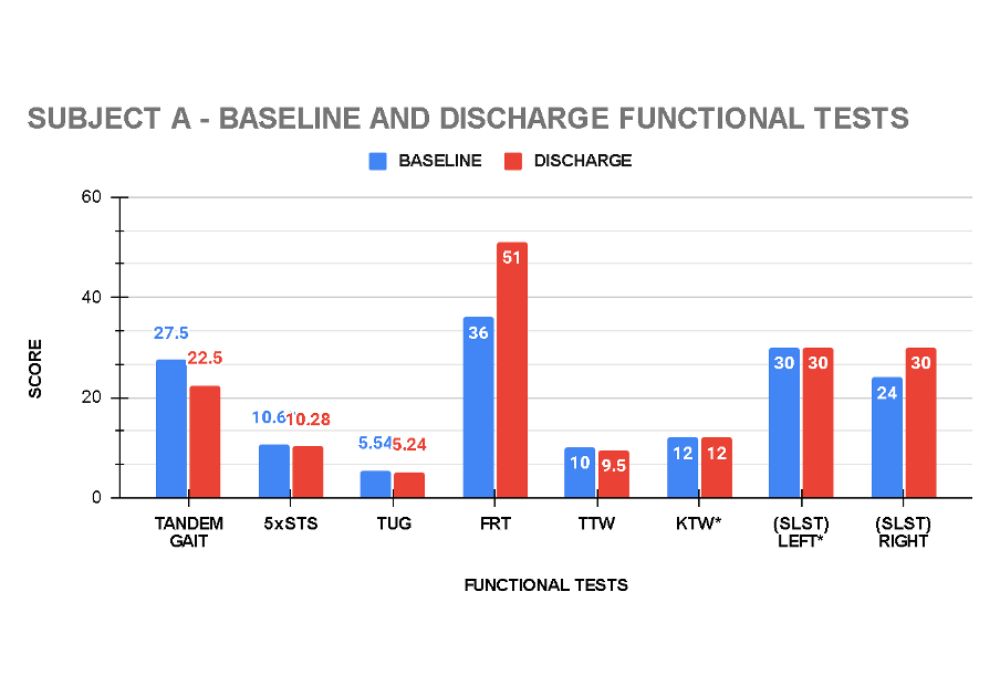
In addition to the Bone Mineral Density tests, 2 clients, (A and D) had functional measurements taken at baseline and at the conclusion of their exercise programme.
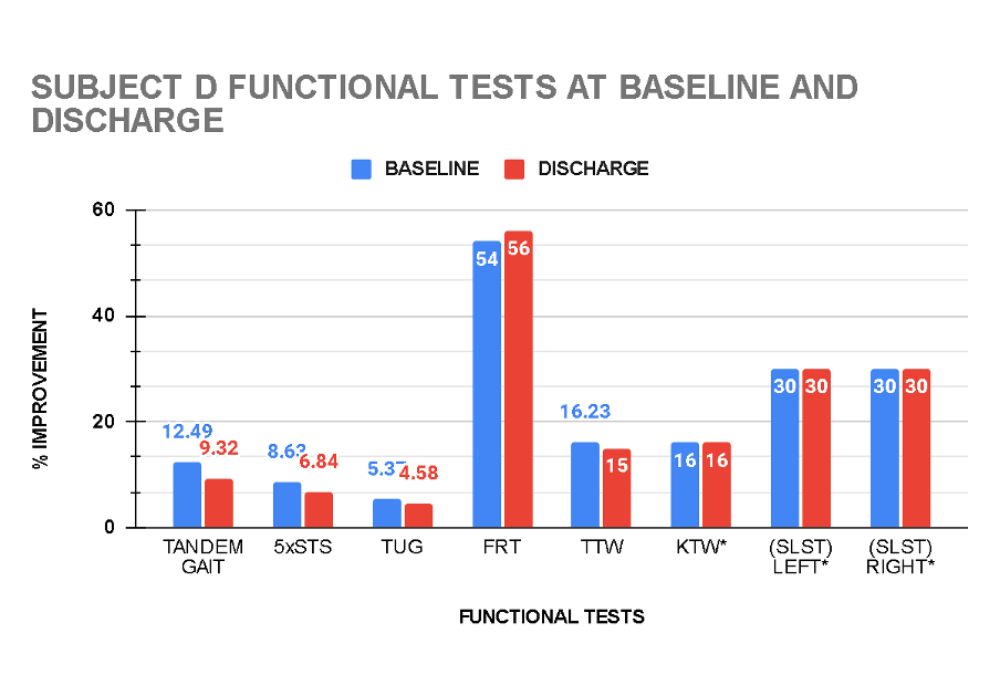
Graphs 7 and 8 show the functional measurements at baseline and at discharge of Subjects A and D respectively.
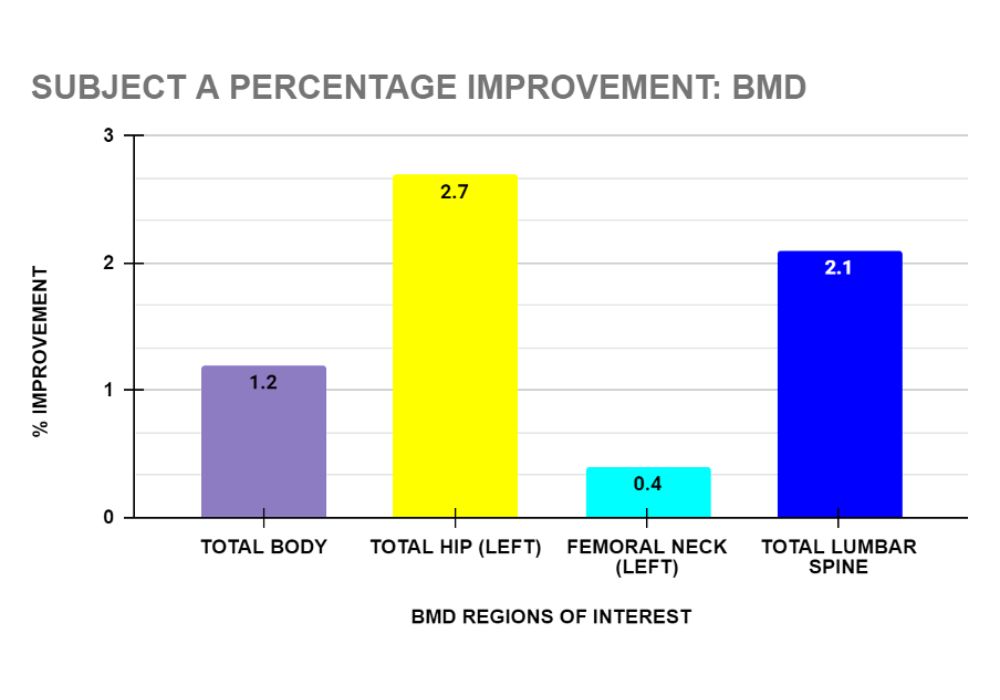
PERCENTAGE IMPROVEMENT OF BONE MINERAL DENSITY
All four subjects recorded improvements post exercise intervention in their Bone Mineral Density, ranging from 0.4 % to 30.4%.
Client A: After 38 sessions over 38 weeks, Subject A’s DXA showed improvement in her BMD in the following regions of interest: total body 1.2 %, total hip (left) 2.7%, femoral neck (left) 0.4% and total spine 2.1%. (see graph 9)
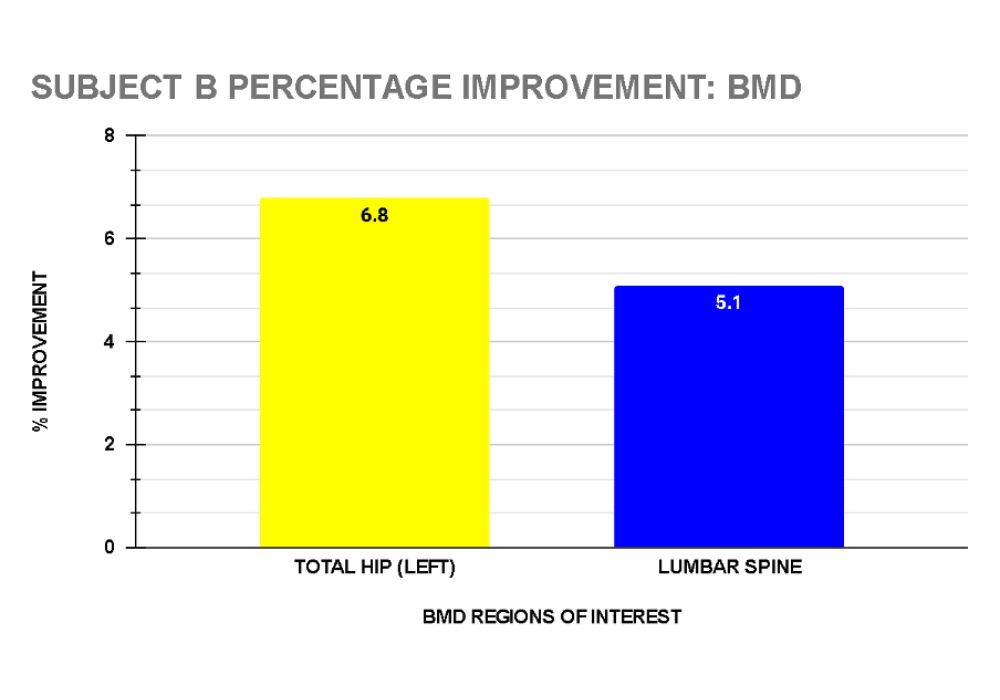
Client B: Following 78 sessions over 78 weeks, Subject B’s DXA reported improvement in her BMD in the following regions of interest: total hip (left) 6.76%,and total spine 5.07%. (see graph 10)
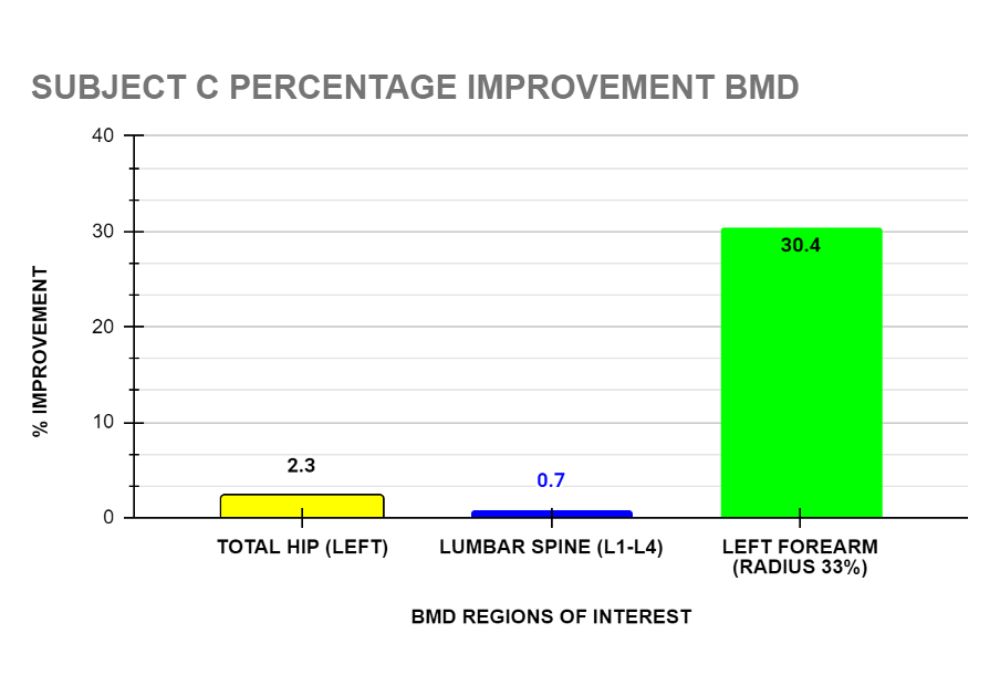
Client C: After completing 16 sessions over 39 weeks, Subject C’s DXA reported improvement in her BMD in the following regions of interest: total hip (left) 2.3%, lumbar spine (L1-L4) 0.7% and left forearm 30.4%. (See graph 11).
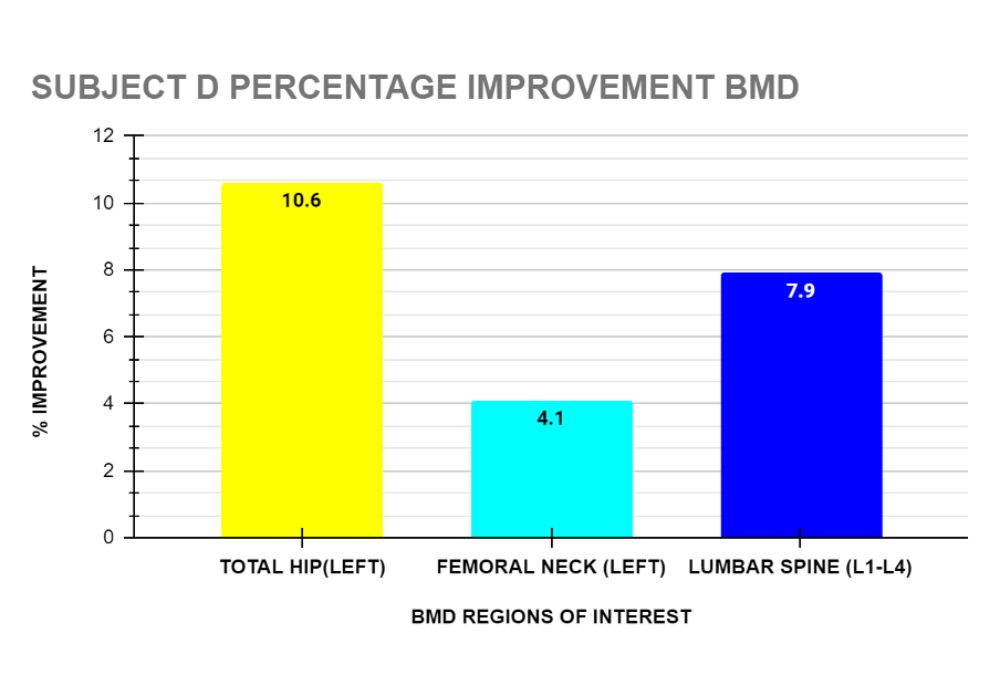
Client D: Following 16 sessions over 22 weeks, Subject D’s DXA reported improvement in his BMD in the following regions of interest: total hip (left) 10.6%, femoral neck (left) 4.1% and Lumbar spine(L1-L4) 7.9% . (see graph 12)
PERCENTAGE IMPROVEMENT IN FUNCTIONAL TESTS
In addition to the Bone Mineral Density tests, 2 clients, (A and D) had functional measurements taken at baseline and at the conclusion of their exercise programme.
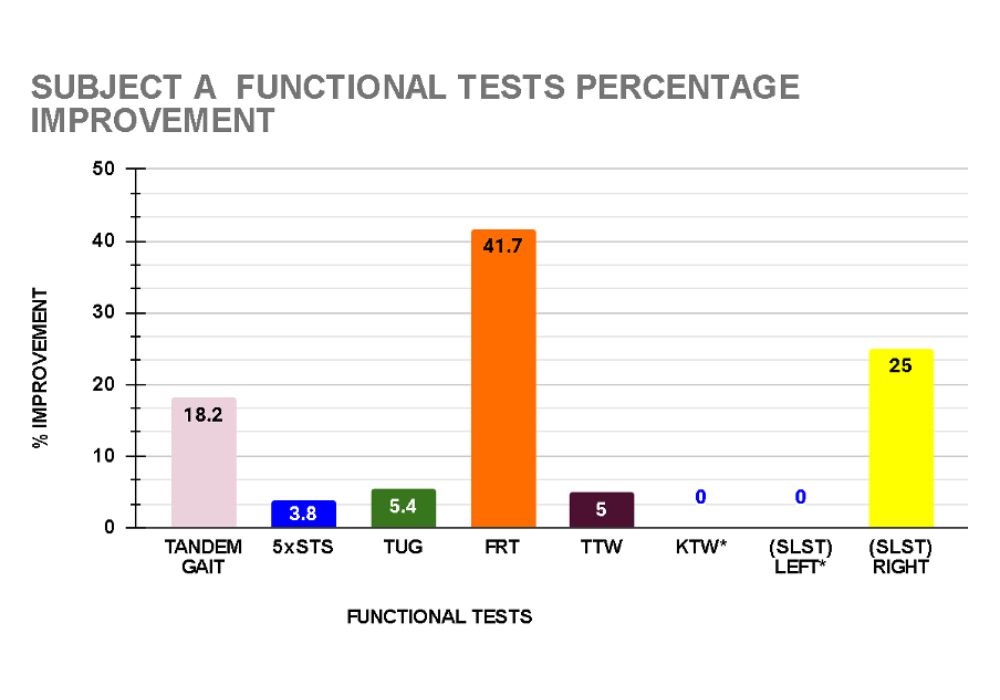
Client A recorded improvement in all functional tests. Balance improved as demonstrated in the tandem gait test (18.2%) and single leg stance test (SLST) right (25%). Dynamic balance, functional mobility and walking ability as measured by the functional reach (FR) and timed up and go (TUG) tests improved by 41.7% and 5.4% respectively. Her tragus to wall (TTW) improved 5% indicating decreased thoracic spine kyphosis. Back and leg strength and endurance improved by 3.8 % in the 5 times sit to stand test. (see graph 13)
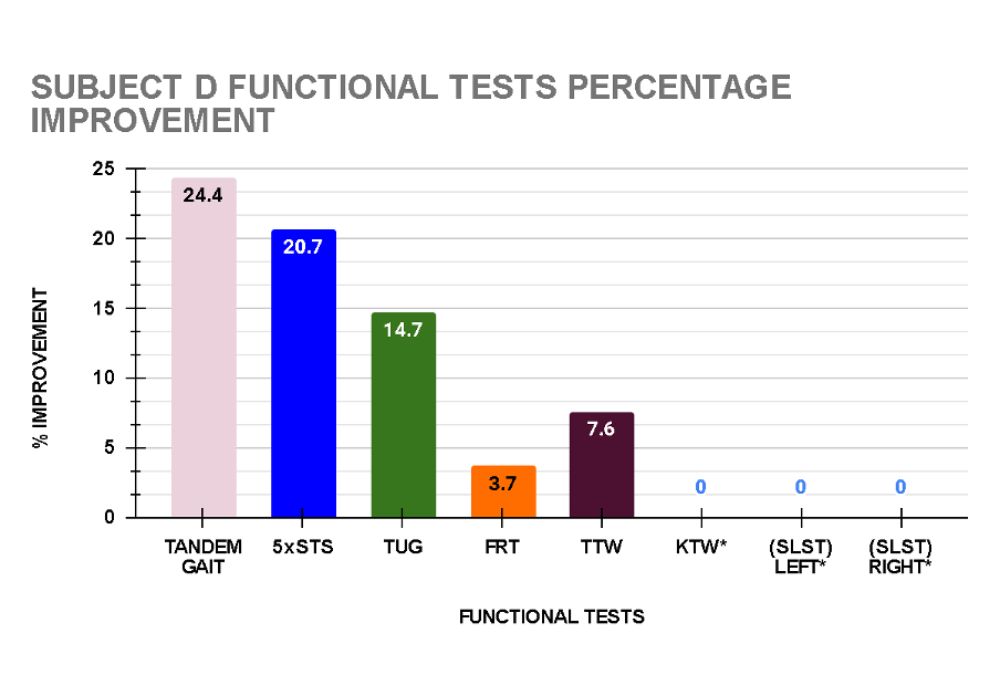
Client D recorded improvement in all functional tests. His balance improved as demonstrated in the tandem gait test (increased by 24.4%). Dynamic balance, functional mobility and walking ability as measured by the functional reach (FR) and timed up and go (TUG) tests improved by 3.7% and 14.7% respectively. His tragus to wall (TTW) increased 7.6% showing an improvement in his thoracic spine kyphosis and the 5 times sit to stand (5xSTS) improved 20.7% indicating increased back and leg strength and endurance. (See graph 14)
Both Subject A and D were tested by the same treating Physiotherapist at baseline and discharge.
DISCUSSION
A Hong Kong study by Kwok et al, 2020⁹ recommends universal DXA testing in women 65 years or over and men 70 years or over. None of our subjects fall into this category but nevertheless were tested and found to be osteopenic or osteoporotic. They commenced Onero™, an exercise programme that includes high-intensity lifts, impact and balance training.
Previous random controlled studies6,7,8 in Hong Kong have tested the effect of exercise on bone density in women and men with a mean age between 60.5 to 73.2 years. Our 4 subjects were considerably younger – with a mean age of 44.5 years. The results represent the first research of the exercise effect of Onero™ on DXA scores in this Hong Kong demographic.
The number of 40-minute sessions varied from 22 to 78 and over a time period varying from 16 to 78 weeks. In the LIFTMOR² study which underpins Onero™, 30 minute group classes were held twice a week for 8 months. Previous studies in Hong Kong6,7,8 have trained subjects from 12 to 24 weeks, 2 times a week for up to 60 to 75 minutes per session, in a group setting. We were not able to provide a group setting due to space constraints, nor could we apply the same “dose” of exercise to each subject due to variable individual capabilities, availability, financial restraints and Covid-19 restrictions.
The 4 subjects varied in presentation with regard to the level of bone loss (osteopenia and osteoporosis), the cause of decreased bone density, age and gender. The positive results in spite of the different characteristics of the subjects suggests that this type of exercise programme may be effective in improving bone health in individuals under the age of 60 years (male and female) with osteoporosis or osteopenia caused by primary or secondary causes.
While the percentage improvement in BMD was positive – ranging 0.4 to 30.4%, a 3 percent change in BMD is considered to be the minimally clinical significant difference (MCID) required. Subject A did not cross the 3% threshold, while Subjects B , C, and D showed improvements above 3% in some if not all ROI’s.
Subject C showed the highest percentage improvement in BMD in her forearm measurement , a 30.4% increase. This large improvement may be due to the increased load through the bones of the upper limb during the overhead press exercise as well as increased muscle contraction around the wrist and elbow when gripping the bar during other lifts. Previous exercise interventions may not have provided enough load through the bones of the upper limb or focussed more on lower limb loading.
Two subjects (A and D) completed the functional tests at discharge. One of the most important areas of treatment in clients with decreased bone density is to decrease the risk of falling due to poor balance, agility, and lower limb strength. Both subjects, while only in their mid 30’s were still able to show improvement in all the functional tests for speed, agility and balance. Currently there is no universally accepted threshold for MCID for the functional tests utilised in this study.
LIMITATIONS
Unlike RCT’s this exercise intervention was not applied in isolation. All clients were encouraged to pursue every avenue possible to improve their bone health. They were provided with information regarding osteopenia and osteoporosis, what constitutes a calcium rich diet, appropriate levels of supplements (for example Vitamin D and Calcium) and we also referred to other specialists such as endocrinologists and dieticians as appropriate. Some clients were also exercising on their own or with personal trainers so the positive effects may have been amplified in their cases.
Due to space restrictions in our clinic we are not able to conduct group classes as in the LIFTMOR and Hong Kong RCT studies. This makes the treatment programme an expensive option.
FUTURE
Future research will be aimed at providing Onero™ to the wider community in Hong Kong, improving the capture of functional tests to show the various physical improvements and further investigating what is the optimal dose of exercise for this demographic.
CONCLUSIONS
This case study series provides preliminary evidence that Onero™ may be effective in improving BMD and functional measurements in women and men with osteopenia or osteoporosis under the age of 60 years of age in Hong Kong. Further research with a larger sample size and a randomised controlled design is warranted to confirm these findings and provide more information regarding the optimal exercise “dose” for this demographic.
ACKNOWLEDGEMENTS
Thank you to the subjects who granted permission to use their data in this presentation and to my colleague Sophie von Burg for her assistance.
REFERENCES
- Koshy F, George K, Poudel P et al (June 16, 2022) Exercise prescription and the minimum dose for bone remodeling needed to prevent osteoporosis in postmenopausal women. A systematic review. Cureus 14(6):e 25993 DOI 10.7759/cureus. 25993.
- Watson SL, Week BK, Weis L, Horan SA, and Beck BR. (2018). High-intensity resistance and impact training improves bone mineral density and physical function in postmenopausal women with osteopenia and osteoporosis: The LIFTMOR randomized controlled trial. Journal Bone Mineral Research 33(2):211-220.
- Watson SL, Week BK, Weis L, Horan SA, and Beck BR. (2015). Heavy resistance training is safe and improves bone, function and stature in postmenopausal women with low to very low bone mass: Novel early findings from the LIFTMOR trial. Osteoporosis International 26(12) 2885-2894.
- Yu, F, Xia W. The epidemiology of osteoporosis, associated fragility fractures, and management gap in China. Archive of Osteoporosis 2019; Mar 8;14(1):32.
- Sue Seen-Tsing Lo. Prevalence of osteoporosis in elderlywomen in Hong Kong. Osteoporosis and Sarcopenia 2021; 7: 92-97.
- Lam FMH, Liao LR, Kwok TCY, Pang MYC. The effects of a 12-week exercise training program on osteoporotic risk in postmenopausal Chinese women with lower bone mass: a randomized controlledtrial. BMC Musculoskeletal Disorders. 2015;16(1):1-12.
- Tsang WWN, Wong V, Fu SN. Effects of a 24-Week Multimodal Exercise Program on Bone Mineral Density and Physical Function in Chinese Older Adults With Osteopenia or Osteoporosis: A Randomized ControlledTrial. Journal of the American Geriatrics Society. 2018;66(9):1697-1704.
- Cheung CL, Tsang WWN, Fong SSM, et al. A 12-week resistance and aerobic exercise program for elderly women with osteoporotic vertebral fractures: a randomized controlled trial. OsteoporosisInternational. 2020;31(5):925-936.
- Kwok TCY, Law SW, Leung EMF, CHoy DTK, Lam PMS, Leung JCS, Wong SH, Ip TP, Cheung CL. Hip fractures are preventable: a proposal for osteoporosis screening and fall prevention in older people. Hong Kong Medical Journal 2020Jun;(26(3):227-235.
- Stanley Sai-Chuen Hui, Yao Jie Xie, Jean Woo and Timothy Chi-Yui Kwok. Effects of Tai Chi and Walking Exercises on Weight Loss, Metabolic Syndrome Parameters, and Bone Mineral Density: A Cluster Randomized Controlled Trial. Evidence-Based Complementary and Alternative Medicine. 2015;ID 976123.
Written by: Judith Anne Gould

BPhty, University of Queensland, 1987
BPhty(Hons), University of Queensland, 1988
MPhil Hong Kong Polytechnic University, 2001
Registered Physiotherapist (HK & AUS)
Member of the Australian Physiotherapy Association
Judith is the founder of Posture Plus Hong Kong, She has over 35 years of experience in musculoskeletal rehabilitation and holds degrees from the University of Queensland and Hong Kong Polytechnic University.
Throughout her career, Judith has successfully treated a variety of work-related and sports-related injuries, from professional athletes to members of the armed forces in Australia and Saudi Arabia. Since moving to Hong Kong in 1994, she has continued to enhance her expertise by completing Pilates training certifications, training numerous physiotherapists in the Bionketic Exercise Technique (B.E.T), and working as a research assistant at HKPU. She has also formulated and designed the Pilates Plus training programme, which utilizes Pilates equipment to improve how people move in order to prevent or change postural dysfunctions that contribute to pain, discomfort or stiffness.
Judith is passionate about helping her clients achieve optimal physical health and wellbeing through personalized treatment plans and holistic approaches.
About Posture Plus
Let our therapists help you recover faster and maintain your health.
Whether you are having difficulties with a recent or a recurring injury / condition, looking to strengthen your performance, or improve your overall health, our therapists can help you with your recovery and provide education so you can confidently manage your own health. Find out more about our services here.

Leading Physiotherapy Clinic in Hong Kong
Prohealth Posture Plus was established in 2007 with the core business being Pilates Plus – a form of Pilates designed by the founder of Posture Plus – Judith Gould. It has expanded over the years to include therapists from a variety of healthcare backgrounds. We are proud to have a team of highly experienced Physiotherapists, Clinical and Sports Massage Therapists and Osteopaths. This provides a broad combination of techniques and experience which enables us to provide the most appropriate treatment for each individual.

Worldwide Talent
Our clinicians are from all over the world – Australia, United States of America, Canada, Poland, United Kingdom, France as well as Hong Kong. Posture Plus is committed to the continued education of both our staff and clients. Each month a staff member presents an inservice to the clinic regarding a new treatment technique or an unusual condition. Relevant information is then disseminated to our clients via newsletter.

Who Are Our Clients
Our clients range in age from babies to the elderly and anyone in between. We treat the weekend warrior, the busy Mum trying to maintain her fitness, the harried office worker with little time to spare, as well as the elite athlete.
-
Locate Our Clinic
-
Call for an appointment!
-
Feel free to message us!
About Us
Since 2007, we provide high-quality services in physiotherapy, clinical and sports massage therapy, osteopathy as well as the unique Pilates Plus programme which was developed by clinic founder Judith Anne Gould.
If you are having difficulties with any injuries or conditions, our therapists can help you with your rehabilitation. Contact us today and let us help you cover faster and maintain your health.
Contact Details
- 9th Floor, 10 Pottinger Street,
Central, Hong Kong
Additional Links
- Bone Strengthening for Osteoporosis and Osteopenia May 20, 2022
- Bone Strengthening for Osteoporosis and Osteopenia December 15, 2023
- Bone Strengthening for Osteoporosis and Osteopenia December 15, 2023
- 聽過骨質疏鬆症或骨質減少症嗎? December 14, 2023
- Pelvic Girdle Pain November 22, 2023
- Fascia and Myofascial Release November 1, 2023